What You Should Know About Cartilage Injuries
- Whitney Lowe
Introduction
It is common for clients to present with conditions outside the usual muscle-related injuries. We can often help these clients, but sometimes, the issue requires a referral to another healthcare provider.
In this issue, we’ll look at two cartilage injuries that need care by an orthopedic physician. Massage may still play a beneficial role in pain management, however. Understanding these pathologies will help you better determine when an appropriate referral is warranted.
Glenoid Labrum Injury
The first of these cartilage injuries is called a glenoid labrum injury. As the name suggests, this problem affects the glenohumeral joint, frequently described as a ball and socket joint. However, the glenoid fossa (the socket) is relatively shallow. The labrum helps make the socket deeper and aids in joint stability.
The fossa is surrounded by a rim of cartilage called the glenoid labrum. The labrum is composed of fibrocartilage similar to the knee’s meniscus. It can be torn, chipped, or cracked, and blood supply is generally poor, so it often takes a long time to heal when injured.
The glenoid labrum is fibrously connected to the glenoid fossa but also has other important soft-tissue attachments. Along the superior margin of the shoulder joint, the tendon from the long head of the biceps brachii attaches to the supraglenoid tubercle. However, it blends into the labrum before inserting into the bone (Image 1). As a result, very high tensile loads generated by the biceps brachii muscle are transmitted to the upper margin of the labrum.
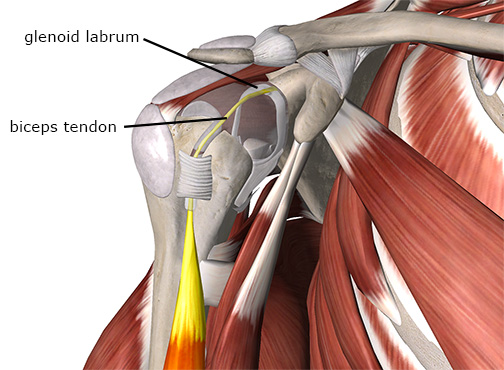
The biceps tendon attaches to the scapula through the labrum.
Image courtesy of Complete Anatomy
When the biceps tendon experiences an immediate, strong pull, it lifts the outer rim of the labrum and can tear it away from the central portion. Often, these forces cause a tear in the superior part of the labrum that runs from anterior to posterior (Image 2). This particular injury is often called a SLAP lesion. SLAP stands for Superior Labrum Anterior Posterior (meaning the tear is in the superior portion of the labrum and runs from anterior to posterior).
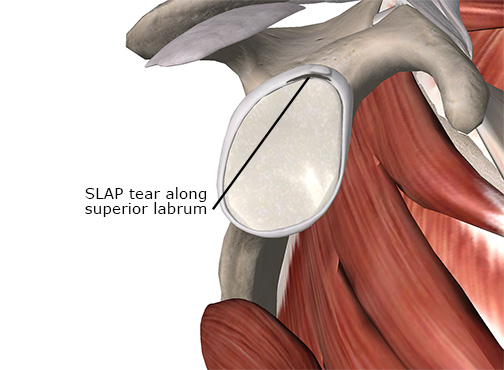
This injury often occurs with a sudden eccentric load on the biceps, such as catching something heavy or a sudden deceleration of the throwing arm. Because the biceps brachii works to decelerate the forceful elbow extension when you throw, it contracts suddenly to stop that motion. This injury is common in athletes like baseball players, whose sports require a lot of throwing.
The SLAP lesion is difficult to identify with physical examination and generally requires high-tech diagnostic evaluation for accurate identification. However, certain clinical signs can indicate the likelihood of a labral injury. The client’s history usually suggests some high force load in the shoulder. There may also be popping or clicking of the shoulder during various motions. Pain may accompany the clicking or popping but is not always present.
The second primary labral injury type is a Bankart lesion or Bankart tear. This injury is a tear to the anterior and inferior portion of the labrum near where it blends with the inferior glenohumeral ligament (Image 3). This portion of the joint capsule and labral complex can also be stressed in repetitive overhead motions, such as throwing or serving a tennis ball. The Bankart lesion is also relatively common with shoulder dislocations.
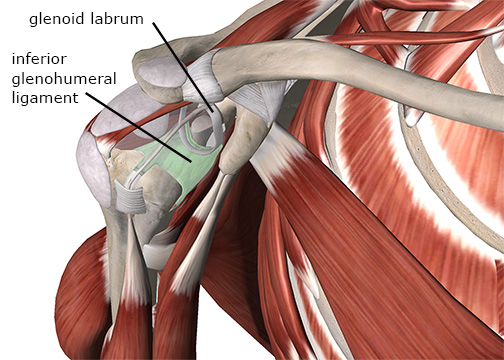
Bankart lesion on the inferior glenohumeral region.
Image courtesy of Complete Anatomy
Falling on an outstretched arm is another common mechanism of labral injury. A labral tear may occur from corresponding joint capsule damage or the humeral head being thrust against the edge of the labrum. In some more traumatic cases, a chunk of bone gets pulled away when the inferior glenohumeral ligament and labrum tear away from the glenoid fossa. This injury is called a Bankart fracture and requires an arthroscopic surgical procedure to repair.
Other complications can develop as a result of labral tears. Because of the poor innervation and circulation to the tissue, the tear may be significantly advanced before the client recognizes the pain.
The labrum holds the humeral head in position, so a tear or disruption in the labral complex can lead to shoulder instability. Increased shoulder instability can predispose the person to dislocations or other shoulder pathologies such as impingement or rotator cuff pathology.
If you suspect a labral injury, the best protocol is to refer the client to an orthopedic physician to diagnose the injury and initiate treatment (often surgery).
Osteochondritis Dissecans
The second cartilage injury to be aware of is called osteochondritis dissecans. It can occur in several locations but is most common in the knee. Knee cartilage injuries commonly involve the knee’s lateral and medial menisci. However, osteochondritis dissecans is different because it is associated with the articular cartilage at the tibiofemoral joint, not the meniscal fibrocartilage between the bones.
Osteochondritis dissecans (OCD) is not a common condition. It is, however, something that the massage practitioner should be aware of as a possible cause of knee pain. OCD is most often seen in younger patients, generally between 13 and 21 years old, and is present in males more than females.
A layer of hyaline cartilage covers the tibia and femur on their ends, reducing friction and wear at the joint. In OCD, a section of hyaline cartilage (and sometimes the underlying bone, called subchondral bone) separates from the remainder of the deeper bone. This separated fragment can float freely within the joint, causing locking, pain, clicking, or crepitus during movement.
The lateral side of the femur’s medial condyle is commonly affected in OCD. During various knee motions, repetitive contact of the medial condyle against the tibial spine causes irritation (Image 4). The tibial spine is a slight ridge of bone on the tibial plateau where the anterior cruciate ligament attaches to the tibia.
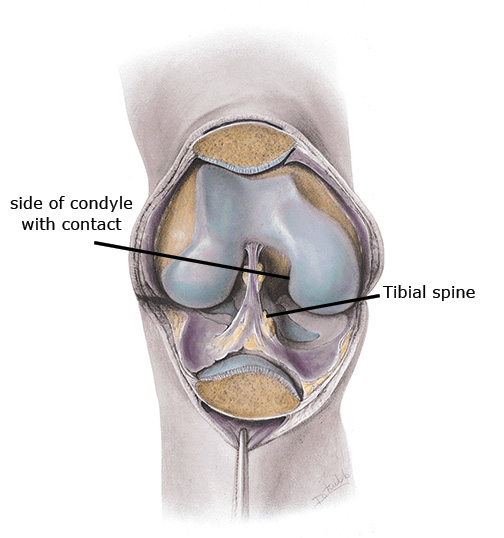
Contact points in the knee leading to OCD.
Mediclip image copyright (1998) Williams & Wilkins. All Rights Reserved.
How cartilage degeneration and separation from the bone starts in OCD is unknown. It can occur from previous trauma, repetitive impact loading, or abnormal ossification of the bone. In addition, the tensile forces of the cruciate ligament attachment may pull on the bone enough to weaken the osteochondral interface. Most likely, it is due to multiple causes. In some cases, avascular necrosis may develop and precede cartilage separation. Avascular necrosis occurs when the blood supply to an area decreases for some reason, resulting in local tissue damage and tissue death (necrosis).
A normal medial meniscus is somewhat round when someone is very young, then it opens up into a C shape with age. A discoid meniscus refers to the shape of the meniscus and retains more of its round or O shape. The O shape can affect how the femoral condyle tracks with the meniscus. A discoid meniscus can contribute to the development of OCD. MRIs have shown meniscal damage in patients with OCD.
It is easy to mistake OCD for other problems; X-rays or MRIs are the most reliable tests. There are other signs and symptoms, however. With active or passive range of motion in the knee, clicking or crepitus may be evident with flexion or extension. Pain may occur along with the clicking movements if a loose piece of cartilage floats in the knee. The client will describe the pain as deep within the knee joint.
Other knee complaints have similar symptoms and should be considered. Meniscal tears, internal ligament sprains, and injury to the coronary ligaments that hold the menisci in place may produce pain felt deep in the joint, similar to OCD. Chondromalacia patellae may also cause crepitus and grinding sensations during knee movements. Patellar tracking disorders and osteoarthritis are also likely to cause diffuse anterior knee pain similar to that of OCD.
Most patients with osteochondritis dissecans are young. Conservative treatment with this population is often effective because they are skeletally immature, and activity modifications can reduce biomechanical stresses. With older patients, conservative treatment appears to be less effective, and there is a greater likelihood that surgery will be necessary.
Conservative treatment often includes patellar taping and exercises for the vastus medialis obliquus muscle. The primary goal is to improve knee joint biomechanics, which decreases aggravation of the osteochondral lesion.
Surgical procedures for OCD are primarily arthroscopic. That means there will be minimal irritation and a quicker recovery. Chondroplasty is the preferred procedure and involves removing the damaged cartilage. However, there may still be pain and crepitus with movement in some cases. In addition, with the cartilage removed, there is a greater chance that the individual will develop osteoarthritis later in life due to friction between the joint surfaces.
To Massage or Not?
The first question to answer is whether massage can cause an adverse effect. With labral tears, there is no indication that massage or gentle range-of-motion activities performed within normal limits would cause a problem or worsen the condition.
The next question is if massage could help treat the injury. Not only are labral tears too deep to access, the labrum is cartilage, so it doesn’t respond to soft-tissue treatment. However, massage can still be beneficial. Dysfunctional mechanics frequently accompany labral tears at the joint. Myofascial trigger points or other biomechanical imbalances can occur as the shoulder compensates for pain, instability, or loss of function. Massage will help restore these biomechanical imbalances and generally help relieve pain.
Understanding labrum pathologies will help you know when they might be occurring and when to get the client referred. However, there does not appear to be anything in the etiology of OCD that suggests massage can be harmful or contraindicated as long as it is performed within comfort limits. Local and specific massage to the knee joint is beneficial in reducing soft-tissue pain in the region. It is still unclear if massage would restore or improve blood flow in the area. However, massage has general pain relief benefits outside of the specific condition treatment.
Therapists should refer clients exhibiting OCD signs to a physician as soon as possible so the condition can be evaluated and treated. Time is an essential factor in getting good results from treatment. The longer joint microtrauma persists, the greater the potential damage in the region. Once the condition is diagnosed and treatment initiated, massage is an excellent adjunct that can help prevent further complications and contribute to treatment success.

