The Long and Winding Nerve
- Whitney Lowe
Introduction
Upper extremity nerve entrapment encompasses more than just carpal tunnel syndrome (CTS). While CTS often dominates discussions about nerve entrapment, numerous other nerve compression syndromes cause significant pain and dysfunction in the upper extremities. One such overlooked condition is long thoracic nerve compression.
Anatomical Background
The long thoracic nerve (LTN) is predominantly a motor nerve and follows a complex path from its origin to its termination, innervating the serratus anterior muscle. It originates from nerve roots between C5 and C7. These root fibers merge after exiting the cervical vertebrae to form the LTN’s main trunk. The nerve then courses between the anterior and middle scalene muscles, closely neighboring the brachial plexus fibers (Image 1).
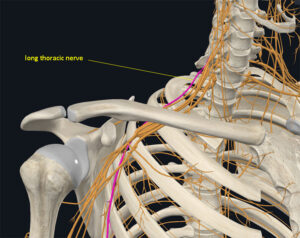
Courtesy of Complete Anatomy
After passing between the scalene muscles, the LTN travels between the clavicle and first rib, then down the lateral rib cage to innervate the serratus anterior muscle. Because it follows such an extensive path, it is vulnerable to compression or traction injuries at multiple locations.
The LTN’s primary function is to provide motor innervation to the serratus anterior, a muscle crucial for shoulder mechanics. The serratus anterior muscle plays two key roles: it holds the scapula against the thoracic rib cage and assists in upward rotation of the scapula. When nerve impingement interrupts motor stimulus to the serratus anterior, it often results in scapular ‘winging’ in which the scapula pulls away from the ribcage. Winging can significantly impact shoulder biomechanics.
LTN compression is commonly a component of scapular dyskinesia, an abnormal position or motion of the scapula. The serratus anterior’s importance in scapulothoracic mechanics cannot be overstated. Later, we’ll explore how muscle weakness due to nerve impingement affects overall shoulder function and movement patterns.
Pathology of Long Thoracic Nerve Injuries
LTN dysfunction primarily results from compression or tension injuries, with compression being more common. Compression injuries may affect the LTN at various locations. At the cervical spine, herniated discs, bone spurs, or tumors can compress the nerve roots. Further along the nerve’s path, compression commonly occurs between the anterior and middle scalene muscles, often in conjunction with brachial plexus compression (thoracic outlet syndrome). External factors like heavy shoulder straps, falls, or direct blows to the shoulder or neck can also compress the nerve in this region.
Tension injuries typically result from sudden lateral neck flexion to the opposite side. This type of injury is seen in contact sports or whiplash injuries. Activities with strong single-arm dominance, such as bowling or tennis, are also associated with LTN injuries. Notably, both activity and prolonged inactivity in awkward positions can lead to nerve compression.
Surgical procedures present another risk factor for LTN injury, leading to compression or tension injuries. These injuries can occur due to how the patient is positioned during lengthy surgeries or from direct trauma during procedures like mastectomies, rib resections, or spinal fusions.
Anatomical variations can also increase susceptibility to LTN pathology by reducing nerve mobility. One such variation occurs when two nerve trunks have a smaller nerve that spans between them. This anomaly is called a connecting or communicating branch. It usually carries fibers from the same nerve roots as the main nerves it connects.
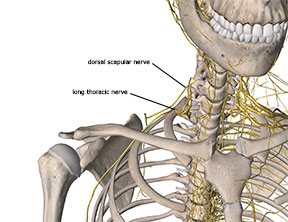
Image 2:
Proximity of long thoracic nerve to dorsal scapular nerve.
Image courtesy of Complete Anatomy
-
Biomechanical Implications of Long Thoracic Nerve Dysfunction
LTN dysfunction significantly impacts shoulder biomechanics due to its innervation of the serratus anterior muscle. The serratus anterior’s function extends beyond simply holding the scapula against the rib cage; it plays a crucial role in complex scapulothoracic mechanics.
During shoulder abduction, the scapulohumeral rhythm is a coordinated movement pattern between the scapula and humerus. This movement pattern involves shoulder abduction and scapular upward rotation (a primary action of serratus anterior). The scapulohumeral rhythm describes this pattern as a 2:1 ratio so that for every 2 degrees of humeral abduction, there is 1 degree of scapular upward rotation. This coordinated movement pattern is essential for proper shoulder mechanics with many upper extremity movements.
When LTN compression leads to serratus anterior weakness, it disrupts this delicate biomechanical balance. The resulting limitation in scapular upward rotation reduces the overall abduction range and increases the risk of shoulder impingement. Without proper scapular upward rotation, the humeral head is more likely to contact the acromion during abduction. The contact may damage structures in the subacromial space, such as the bursa, supraspinatus tendon, or joint capsule.
Recognizing Symptoms of Long Thoracic Nerve Pathology
Long thoracic nerve pathology presents unique symptoms because the LTN is primarily a motor nerve. Unlike typical nerve compression syndromes, LTN injuries often lack the sharp pain or paresthesia commonly associated with other upper extremity nerve issues because it doesn’t have many sensory fibers in the nerve.
The primary symptoms of LTN dysfunction include shoulder weakness and potential shoulder pain. The shoulder pain may result from secondary impingement issues caused by biomechanical dysfunction rather than nerve compression. Failing to recognize the LTN’s role in these symptoms can lead to ineffective treatment focused solely on addressing shoulder impingement.
Clients may report difficulty with overhead activities, which heavily rely on scapular upward rotation. This weakness can occur with or without accompanying pain or sensory deficits. The absence of typical nerve compression symptoms makes LTN pathology easy to overlook. The challenge in recognizing LTN emphasizes the importance of a thorough assessment of shoulder biomechanics. One of the more effective ways to see potential motor impairment of the LTN is to watch the client’s active shoulder abduction movement and see if they can get full shoulder abduction smoothly (good scapulohumeral rhythm) and without apparent compensation.
In a future post, we’ll explore more assessment protocols and beneficial treatment strategies for addressing LTN compression. You can learn more about LTN nerve pathology in our comprehensive orthopedic medical massage Cervical course. Gain in-depth knowledge and detailed videos while earning 12 CE credits!
Resources:
- Keenan KE, Skedros JG. A patient with clavicle fracture and recurrent scapular winging with spontaneous resolutions. Case Rep Orthop. 2012;2012:603726. doi:10.1155/2012/603726.
- Oma N, Alvi F, Srinivasan MS. An unusual presentation of whiplash injury: long thoracic and spinal accessory nerve injury. Eur Spine J. 2007;16 Suppl 3:275-277. doi:10.1007/s00586-007-0413-z.
- Skedros JG, Phippen CM, Langston TD, Mears CS, Trujillo AL, Miska RM. Complex Scapular Winging following Total Shoulder Arthroplasty in a Patient with Ehlers-Danlos Syndrome. Case Rep Orthop. 2015;2015:680252. doi:10.1155/2015/680252.
- Tsirikos AI, Al-Hourani K. Transient long thoracic nerve injury during posterior spinal fusion for adolescent idiopathic scoliosis: A report of two cases. Indian J Orthop. 2013;47(6):621-623. doi:10.4103/0019-5413.121595.
- Shilal P, Sarda RK, Chhetri K, Lama P, Tamang BK. Aberrant Dual Origin of the Dorsal Scapular Nerve and Its Communication with Long Thoracic Nerve: An Unusual Variation of the Brachial Plexus. J Clin Diagn Res. 2015;9(6):AD01-AD02. doi:10.7860/JCDR/2015/13620.6027.
- Pecina M, Markiewitz A, Krmpotic-Nemanic J. Tunnel Syndromes: Peripheral Nerve Compression Syndromes. Boca Raton: CRC Press; 2001.

