Understanding Glenohumeral Dislocation
- Whitney Lowe
The shoulder (glenohumeral) joint has the greatest range of motion of any joint in the body. Yet, the joint’s bony architecture provides very little stabilizing support. Consequently, the majority of shoulder stability comes from soft tissues that both guide and limit movement at the shoulder. This joints enhanced mobility leaves it vulnerable to problems, in particular when high force loads occur at mechanically disadvantageous positions. One of these issues is a glenohumeral dislocation, in which the humeral head comes out of the glenoid fossa. In these injuries, the shoulder’s restraining soft tissues are unable to maintain the joint in its anatomical location, leading to significant shoulder instability.
Subluxation is another type of injury involving lost glenohumeral stability and movement of the humeral head. A subluxation occurs when the joint has moved partially out of the joint, but not entirely. Subluxation may also refer to a situation in which the bone has moved out of its position in the joint and then moved back in on its own.
Background
Even though it is commonly referred to as a ‘ball and socket’ joint, the glenoid fossa is actually quite shallow (Figure 1). As a result, the humeral head can be dislocated from the glenoid fossa without much effort. There is a rim of cartilage that surrounds the glenoid fossa called the glenoid labrum (Figure 1). This rim of cartilage helps make the fossa a little deeper to protect against dislocations, but they still occur.
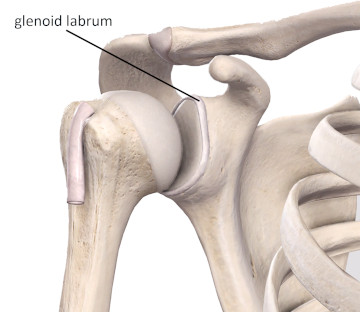
Figure 1
The shallow glenoid fossa and glenoid labrum
Image is from 3D4Medical’s Complete Anatomy application
Most dislocations are anterior dislocations. This means that the head of the humerus moves in an anterior direction relative to the glenoid fossa. The combined motions of abduction and external rotation of the humerus are the motions most likely to produce an anterior dislocation.
Numerous ligaments surround the glenohumeral joint, but they all work together to form the joint capsule. An intact joint capsule with all the ligamentous restraints is shown in Figure 2. The tissue of the joint capsule is often indistinguishable from the ligaments that span the glenohumeral joint. However, anatomists have chosen to name some of these ligament structures separately. One of the most important ligament structures for resisting anterior glenohumeral dislocation is the inferior glenohumeral ligament. In anterior dislocations, this ligament is pulled or stretched beyond its capacity.
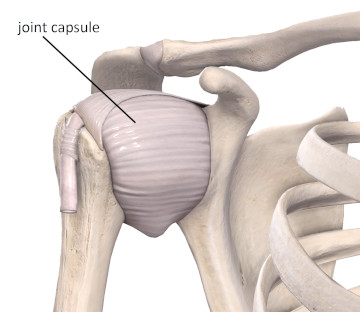
Figure 2
The glenohumeral joint capsule and ligamentous restraints
Image is from 3D4Medical’s Complete Anatomy application
The inferior glenohumeral ligament attaches to the lower border of the glenoid labrum. When the ligament is exposed to excessive tensile stress, it may pull the labrum away from the rim of the glenoid fossa. This is an injury called a Bankart lesion and often accompanies anterior glenohumeral dislocations and becomes a problem that must be addressed once the actual dislocation has been corrected.
Another soft-tissue structure that plays a vital role in preventing anterior dislocations is the biceps brachii long head tendon. This tendon attaches to the supraglenoid tubercle and has fibers that insert into the upper region of the glenoid labrum (Figure 3). Because the tendon courses across the anterior aspect of the humeral head, it helps prevent anterior dislocations of the humerus.
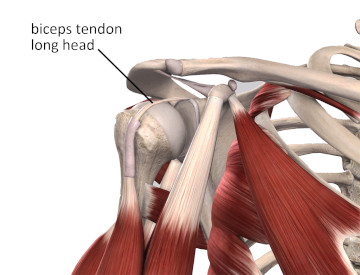
Figure 3
The biceps tendon long head
Image is from 3D4Medical’s Complete Anatomy application
If an anterior dislocation has occurred, the biceps tendon may pull enough on the superior portion of the labrum to pull it away from the upper glenoid fossa. This injury is called a SLAP lesion, which is an acronym for Superior Labrum Anterior Posterior. It indicates a tear to the superior aspect of the labrum running in an anterior to posterior direction. If a SLAP lesion has occurred it is likely to make the biceps brachii much less effective in holding the humeral head in its proper position. Consequently, there is less stability in the joint and future dislocations are even more likely.
Instability is one of the prime factors that both causes dislocations and results from them. For example, when a dislocation or subluxation has occurred, the ligaments and joint capsule are likely to be somewhat overstretched. Once these structures are overstretched, the head of the humerus is prone to moving around more than it should in the glenoid fossa, and this creates instability in the joint. The more instability in the joint, the higher is the chance of future dislocations and additional problems.
Several other problems may result from shoulder instability or a history of glenohumeral dislocation. Continued instability can cause osteoarthritis as the client ages. Also, conditions such as shoulder impingement syndrome may develop. When the humeral head is moving around more in the glenoid fossa, there is a higher chance for it to press the soft tissues that are above it against the underside of the acromion process or the coracoacromial ligament. Damage to the supraspinatus, joint capsule, biceps tendon long head, or sub-acromial bursa may occur.
Assessment and Treatment Considerations
Most shoulder dislocations happen as a result of a sudden traumatic injury or forceful motion of the shoulder. Signs that these tissues are at issue include the client holding the arm close to the body to prevent upper extremity movement. A sulcus sign (slight divot under the acromion process on the lateral shoulder) may also be evident when the arm is in a neutral position. The sulcus sign indicates the humeral head has dropped from its normal position and is out of position. If an individual has a history of a traumatic injury to the shoulder and is showing a sulcus sign, they should immediately be referred to a physician for diagnosis and correction of the dislocation.
One of the most common methods of recognizing a potential problem with dislocations or shoulder instability is the apprehension test. In the classic apprehension test, a client shows either verbal or visual apprehension when the shoulder is moved into a position close to where the dislocation previously occurred. For example, if the client suffered an anterior dislocation from an extreme of abduction and external rotation, they are likely to show great apprehension if their arm is moved near the end range in abduction and external rotation. Recognizing this sign is of utmost importance as you may be conducting various range of motion or stretching techniques and not realize that you are getting near a region of significant instability for your client’s shoulder.
Correcting a dislocated joint should only be done by someone skilled and trained to reduce dislocations, such as an orthopedist or physical therapist (this treatment is out of the scope of practice for massage practitioners). If performed improperly, serious injury can result in attempting to correct a dislocation. The brachial plexus and axillary artery are very close to the lip of the glenoid labrum and can be damaged or severed with an improper attempt to fix a dislocation.
A massage therapist is rarely going to be around right after a dislocation has occurred. More likely, the massage therapist’s role is helping to manage the resultant soft-tissue reactions to the injury. Massage can address soft-tissue challenges such as impingement, tendon irritation, or biomechanical imbalance resulting from the injury.
Identifying previous glenohumeral dislocations in the client history is very important. The client may not realize this is an important piece of information to convey. However, they will likely show unease as you perform movements that involve significant abduction and external rotation, which could potential cause dislocation again. This potentially dangerous situation highlights the crucial importance of taking a thorough and comprehensive history and also of understanding various biomechanical challenges and pathologies that could play an essential role in effective treatment.

