Exploring Elusive Compartment Syndromes
- Whitney Lowe
Many of our clients come in with chronic, aching muscular pain. The natural reaction is to attempt to relieve their pain, often through deep pressure massage applications. However, there are certain conditions in which performing deeper levels of treatment is contraindicated and can actually make the condition worse. Compartment syndromes fall into this category and understanding this orthopedic disorder is very important for the massage therapist because in certain cases it can be an extremely serious injury. A review of some core anatomy principles helps illustrate what a compartment syndrome is and how it develops.
What is a Compartment Syndrome?
Muscles are gathered together in groups and surrounded by fascial walls, bones, or tough interosseous membranes. The space within these anatomical boundaries is called a compartment. Figure 1 shows a cross-section of the lower leg and the compartments are easy to identify in the images with their different colors. There are four separate compartments in the lower leg. The compartments contain not only muscles, but also arteries, veins, nerves, and lymphatic vessels.
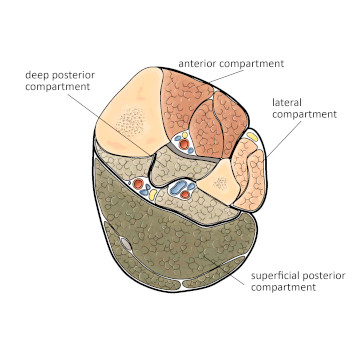
Figure 1
Four compartments of the lower leg
Mediclip image copyright (1998) Williams & Wilkins. All Rights Reserved.
A compartment syndrome occurs when the contents of the compartment expands thereby increasing pressure on all of the structures within the compartment. Chronic overuse or acute trauma can cause inflammation and swelling of the muscles within the compartment and is usually responsible for the increase in compartmental pressure.
As the muscles swell, pressure increases within the compartment and can cut off blood supply or cause permanent nerve damage. Compartment syndromes occur most often in the lower leg, but can also occur in the thigh, hands, forearm, feet, and buttocks, among other regions.1 To better understand how they occur, let’s take a look at the two different types of compartment syndromes: acute and chronic.
Compartment Syndrome: Acute or Chronic
Acute compartment syndromes are less common than chronic, but are far more dangerous. The reason they are more dangerous is they usually involve greater degrees of swelling and consequently greater pressure levels develop within the compartment. Acute syndromes are caused by direct trauma to the compartment, vigorous exercise, blood clots, tight bandaging, or long periods of unusual compression. In cases of direct trauma to the compartment, symptoms may not appear immediately, which can confuse identification of the condition.
An example clinical case report describes a man who passed out on a staircase for 8 to 10 hours as a result of a drug overdose. The prolonged pressure on his thigh and gluteal region from the staircase caused irreversible neurological damage to his sciatic nerve as well as other systemic effects including kidney injury.3 Acute compartment syndromes can also result from long surgeries where a body part is immobile for long periods on the operating table, so medical staff must be careful to prevent constant pressure in one location.
Chronic compartment syndrome, also called exertional compartment syndrome (ECS) is far more common than the acute injury. The most common location to develop ECS is the anterior compartment of the lower leg. ECS occurs when muscles swell as a result of repetitive activity. Symptoms abate when the individual stops the activity.
While the lower leg is certainly the most common location for ECS, it may occur in other regions of the body as well. ECS of the forearm may occur after prolonged activities requiring significant grip strength. The condition is commonly reported in competitive motorcycling where it is known as “arm pump,” but is also reported in gymnastics, hockey, wheelchair athletics, climbing, waterskiing, and kayaking.4
A recent study reported on a thigh compartment syndrome that occurred eight days after a soccer trauma. The man affected was hit on the thigh during a soccer game, causing severe edema of the vastus intermedius. This swelling eventually led to a thigh hematoma 8 days later, that developed secondary to the rupture of the profunda femoris vein. The tissue damage was deep enough not to be immediately apparent after the incident.2
Symptoms
It can be difficult to accurately identify a compartment syndrome just by physical examination alone. However, there are some key characteristics. Other than a rapid vs. slow onset, symptoms of acute and chronic compartment syndromes are pretty similar. In some acute compartment syndromes the symptoms are more pronounced because the compartment pressures are greater.
Pressure on vascular structures can cause discoloration of the limb or coldness in the extremity. Lack of venous return can also cause sensations of tightness or fullness of the extremity that are different from those of chronic muscular overuse. Neurological sensations, such as paresthesia, numbness, or weakness are likely to result from compression of motor and sensory nerves. These neurological sensations are generally not present with chronic muscular overuse conditions like shin splints so this is a helpful way to distinguish the compartment syndrome from shin splints in the lower leg.
Complaints of aching or cramping in the affected muscles is common. In chronic cases these symptoms occur within about a half an hour after starting exercise. Symptoms often persist throughout the exercise, and then gradually subside once the activity is stopped. In the lower leg it is common for compartment syndrome to occur after a history of other lower extremity dysfunction such as shin splints.
The most accurate way to determine the presence of compartment syndrome is through the use of an intra-compartmental pressure reading. This procedure is performed by a physician who inserts a special needle into the compartment that can read the intra-compartmental pressure. Once it is determined that a compartment syndrome exists there are different strategies for treatment depending on the severity of the compartmental swelling. Keep in mind that it will be difficult to identify a non-aggravated compartment syndrome with a compartmental pressure reading if the needle pressure reading is performed well after the exercise induced trauma has subsided.
Treatment Strategies
Treating acute compartment syndrome involves an emergency procedure to decrease compartmental pressure; delaying this procedure can cause irreversible tissue damage. This is one instance in which RICE (Rest, Ice, Compression, & Elevation), the common method for treating an acute injury, is actually a bad idea. Rest is certainly beneficial, but ice can cause decreased tissue fluid movement and that is not helpful for reducing compartmental pressure. It should be pretty obvious that additional compression is also a bad idea for a condition where excess compression is causing tissue damage. Elevation could also impair return of needed circulation.
In the case of an acute compartment syndrome an emergency surgery called a fasciotomy may be performed. In this procedure, the surgeon cuts a slit in the fascial wall, and lets the contents of the compartment bulge through until they can subside in size back to their normal state. If the intracompartmental pressure is not relieved in an acute condition, permanent tissue damage can result.
Chronic compartment syndromes are often treated with various activities that help reduce the cumulative overload on the muscle. Stretching and various exercises are commonly used in physical therapy to address the ECS.
Massage Strategies
One of the key questions that emerges for the soft-tissue therapist is what role massage might play in addressing this condition. Massage generally increases pressure on the tissues being treated so this is an important consideration with compartment syndrome.
The key to using massage as a treatment for ECS is that it can be very effective in helping to reduce the chronic muscular tension that led to the condition. However, treatment should not be applied while symptoms are aggravated. For example, if a person has just gotten through running and is complaining of aching pain in her lower legs, this is not the time to do the treatment. On the other hand, if she is consulting you three days after her last run and the pain has subsided, at this point massage would be appropriate.
Massage for a compartment syndrome should always be applied within the client’s pain tolerance and it is important to make sure that it does not aggravate any of the existing vascular or neurological symptoms that would indicate increasing pressure in the compartment. Of course, an obvious and most important factor in the treatment of any compartment syndrome is finding a way to reduce the offending activities that have led to the chronic overuse to begin with.
References
- Via AG, Oliva F, Spoliti M, Maffulli N. Acute compartment syndrome. Muscles Ligaments Tendons J. 2015;5(1):18-22.
- How MI, Lee PK, Wei TS, Chong CT. Delayed presentation of compartment syndrome of the thigh secondary to quadriceps trauma and vascular injury in a soccer athlete. Int J Surg Case Rep. 2015;11:56-58.
- Panagiotopoulos AC, Vrachnis I, Kraniotis P, Tyllianakis M. Gluteal compartment syndrome following drug-induced immobilization: a case report. BMC Res Notes. 2015;8:35.
- Harrison JWK, Thomas P, Aster A, Wilkes G, Hayton MJ. Chronic exertional compartment syndrome of the forearm in elite rowers: a technique for mini-open fasciotomy and a report of six cases. Hand (N Y). 2013;8(4):450-453.

