Biomechanics of Tendon and Ligament Tissue
- Whitney Lowe
Updated 01-24-24
While massage therapists may focus on muscles to treat pain and injuries, tendons and ligaments, and other vital soft tissues, significantly contribute to musculoskeletal disorders. Understanding tendon and ligament anatomy, their mechanics, and how they are injured is crucial for devising effective treatments.
In this issue, we explore the essential aspects of tendon and ligament structure that affect their function and susceptibility to injury.
Structure and Function
Tendons and ligaments, both made of dense regular connective tissue, have crucial differences. Tendons link muscle to bone, while ligaments connect bone to bone. This distinction is vital but may cause confusion. For instance, the patellar tendon, which starts from the quadriceps and attaches to the tibial tuberosity, encompasses the patella – a sesamoid bone within the tendon. Despite this, many anatomical texts label the section between the patella and tibial tuberosity as the patellar ligament, as it connects two bones: the patella and the tibia (Image 1).
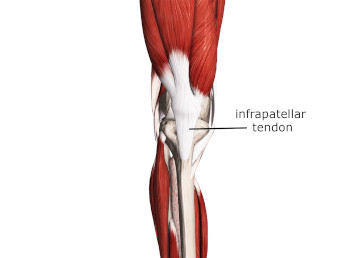
Infrapatellar tendon is often listed as the patellar ligament because of its connection between the patella and tibia.
Image courtesy of Complete Anatomy.
Understanding the structure and function of connective tissues is crucial, rather than focusing solely on their anatomical connections. The tissue extending from the quadriceps to the tibial tuberosity functions as a tendon, not a ligament, even though it incorporates the patella. Its fibrous composition is distinctly tendinous.
A tendon’s primary role is transmitting muscle contraction force to the bone, minimizing tensile force loss. The tendon achieves effective force transmission through parallel aligned collagen fibers. The parallel alignment provides maximum tensile strength against forces along these fibers’ orientation (Image 2).
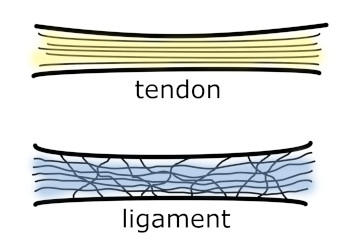
Collagen fibers in the tendon are much more parallel aligned. In ligament they are looser and also run in multiple directions.
The parallel orientation of tendon fibers makes them stiff, allowing them to transmit muscle contraction effectively, akin to a wire rather than a rubber band. This stiffness is why tendon tears are less common than muscle tears in strain injuries.
Tendons usually face forces in a single direction, but in some areas, like the hand’s finger flexors and extensors, tendons experience multidirectional tensile loading. Here, lateral connections between tendons form a network, aiding finger movement coordination by maintaining tendon spacing and force distribution.
Furthermore, some tendons are encased in a synovial sheath, particularly in distal extremities, where they make sharp turns near joints. This sheath, held close to the joint by a retinaculum, primarily reduces friction during movement (Image 3).
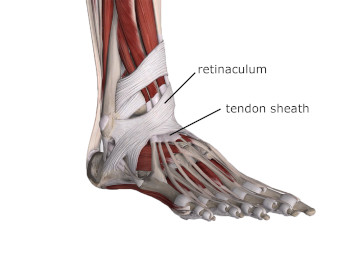
Tendon sheaths and their binding retinacula.
Image from 3D4Medical’s Complete Anatomy.
Tendons are designed for force transmission, while ligaments primarily ensure skeletal stability by connecting bones and guiding joint movements. This guidance helps maintain optimal joint surfaces and reduces wear from friction during movement and weight bearing.
Ligaments are typically smaller and shorter than tendons, usually spanning only one joint. Their close attachment points are crucial for movement guidance and joint stability. Like tendons, ligaments have collagen fibers primarily oriented in parallel but also contain multiple-direction fibers. This structure suggests that while ligaments mainly resist force in one direction, they can also withstand multidirectional forces.
Ligaments have a higher elastin content than tendons, giving them greater pliability to absorb joint loads with some flexibility. Unlike tendons, ligaments don’t require synovial sheaths since they don’t cover multiple joints or experience the same sliding movements as tendons.
Common Pathologies
Tendon injuries often result from repetitive loads over time. Ligament injuries usually result from sudden, high-force loads. Let’s examine these injury processes. Tendinitis, a well-known tendon disorder, was once thought to be inflammatory. However, recent research suggests little to no inflammation in these cases. Instead, overuse may lead to structural breakdown of the collagen matrix within the tendon. Thus, terms like tendinosis or tendinopathy, indicating pathology without implying inflammation, are now more appropriate.
Treatment strategies differ based on whether tendon damage is degenerative or inflammatory. Anti-inflammatory treatments like corticosteroid injections can impair collagen synthesis and weaken tendons. Consequently, that treatment might make the tendinosis worse.
The exact cause of pain in non-inflammatory tendon disorders is unclear, but one theory involves chemical irritation activating nociceptors in tendons. Mechanical overload is a primary cause of tendon pathology, but other factors like fluoroquinolone antibiotics can also impact tendon integrity. Understanding a client’s history with these antibiotics is crucial, as treatments increasing tendon load might not be suitable.
Tenosynovitis, another tendon condition, is an inflammatory disorder affecting tendons within a synovial sheath. Chronic overuse can lead to inflammation and adhesions between the tendon and their sheath and lead to pain and movement difficulty.
Ligament injuries, or sprains, occur from excessive force loads and are measured in three grades: mild, moderate, and severe. Ligaments, with their multidirectional fibers and higher elastin content, can endure some sudden stretch. However, excessive force can cause permanent elongation or rupture, leading to various pathologies like joint instability or osteoarthritis.
Check out this video below for additional ideas on discriminating between tendon and ligament injuries.
Orthopedic Medical Massage Treatment Strategies
Identifying ligament and tendon injuries is vital to crafting effective treatments. For both tendon and ligament injuries, gentle, protected movement is now favored over immobilization, as movement promotes faster healing.
Treating chronic tendon overuse involves a somewhat paradoxical approach. While some rest is beneficial, applying specific loads, particularly eccentric muscle loads, can hasten recovery. This counterintuitive strategy helps the tendon adapt and heal despite overuse causing the injury.
For massage therapists, the role of massage in treating these injuries is a topic of ongoing research. Deep friction massage, previously used to address tendon scarring, may still be effective for collagen degeneration. Some research suggests that massage could stimulate fibroblast activity, aiding tendon repair.
Friction massage is also helpful for tenosynovitis. Some suggest it may reduce adhesions between the tendon and its sheath, although research has not verified this model. Treating associated muscles is crucial for any tendon pathology. Various massage techniques can reduce muscle tightness, thereby lessening tensile load on the tendon.
For ligament sprains, massage’s role in treatment is less clear but may aid in tissue regeneration and prevent adhesions that limit motion. Regular friction massage, including self-massage, could be beneficial. It’s vital to remember that ligaments, lacking contractile tissue, do not contract or release. Techniques aimed at “releasing” ligaments are misguided, as ligaments don’t release since they have no contractile elements.
It is essential to understand the functions of soft tissues, their injury mechanisms, and how massage interacts with these injuries. As knowledge of tendon and ligament physiology grows, so will our ability to develop more effective treatment strategies, helping clients return to activities sooner.
Want to learn more about identifying various soft-tissue disorders so you can be more effective in treatment? Check out our assessment cheat sheet at:

