Exploring Elusive Knee Pain: The Synovial Plica
- Whitney Lowe
Massage therapy is highly effective for managing many soft-tissue pathologies. However, some conditions may closely mimic more common issues but fail to respond to standard treatment approaches. A prime example is synovial plica syndrome, a knee disorder frequently misdiagnosed due to its resemblance to other common knee pathologies.
What is a Synovial Plica?
During embryological development, tissues gradually differentiate into their mature forms. Early in fetal growth, tissue bands separate the knee into distinct compartments. As the knee joint matures, these bands typically diminish and are eventually encapsulated by the synovial capsule. In some individuals, however, these embryonic tissue bands persist into adulthood, forming tissue folds known as synovial plicae.¹
The medial knee region is one of the most common sites for a symptomatic plica, termed medial plica syndrome. While a plica may exist without symptoms throughout life, it can become problematic due to chronic overuse, direct trauma, or secondary injuries, resulting in swelling and fibrosis. Repetitive knee movements generate friction, causing the plica to stiffen and lose flexibility. Occasionally, a fibrotic plica may bowstring across bony prominences, aggravating symptoms.
Other factors contributing to plica irritation include direct trauma, excessive twisting of the knee, or intra-articular bleeding or effusion secondary to another knee injury. Secondary dysfunctions, such as meniscal tears, may complicate diagnosis. Rarely, the plica can become calcified, significantly exacerbating pain and altering knee mechanics.²
Once fibrotic, the plica may become pinched between the femur and patella during knee extension, with the medial aspect being most susceptible (Figure 1). The medial patellar plica lies beneath the distal portion of the vastus medialis, specifically the Vastus Medialis Obliquus (VMO). Notably, VMO pain commonly associates with patellar tracking disorders, complicating accurate diagnosis and potentially masking synovial plica involvement.¹
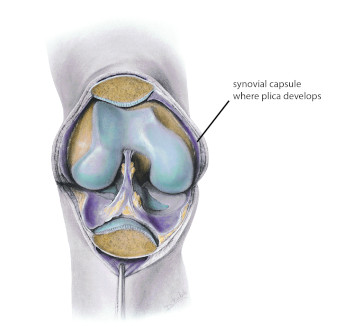
Figure 1
The knee opened up to show location of plica development
Mediclip image copyright (1998) Williams & Wilkins. All Rights Reserved.
The knee opened to show location of plica development
Mediclip image copyright (1998) Williams & Wilkins. All Rights Reserved.
Over time, fibrotic changes in the joint can lead to softening and degeneration of patellofemoral cartilage, suggesting a possible causal relationship between synovial plica syndrome and chondromalacia patellae.¹
Evaluating the Synovial Plica
Diagnosing synovial plica syndrome is challenging due to symptom similarity with other knee conditions. However, characteristic indicators may aid identification. The primary symptom is intermittent, dull, aching pain medial to the patella, typically aggravated by activities involving forceful knee extension, such as rising from a squat.
Sustained knee flexion often exacerbates pain, as the plica becomes taut. Pain generally increases during knee extension movements but decreases once the knee remains fully extended. Patients might also experience sensations of instability, snapping, or clicking, particularly when moving from flexion into extension (Figure 2).

Figure 2
Pain most commonly felt moving from flexion into extension.
Pain commonly experienced moving from flexion into extension
During palpation, general tightness in the knee area, particularly in the quadriceps group, is common. The quadriceps retinaculum fibers often exhibit tenderness due to deep fascial connections with the knee’s synovial capsule. Reducing quadriceps tightness is therefore crucial.
Quadriceps atrophy is a frequent finding in many knee pathologies, including plica syndrome. Evaluate quadriceps atrophy by measuring muscle circumference just superior to the patella, comparing it with the unaffected side.
Occasionally, a palpable band on the medial knee can be detected by rolling the fingers across the region; however, this is not consistently reliable. A more definitive pain provocation test involves holding the knee at approximately 30 degrees of flexion and medially pushing the patella, reproducing pain by pinching the plica between the femur and patella.³ Nonetheless, physical examination alone is not highly reliable, and imaging techniques like MRI are often required for confirmation.
Treatment Approaches
Initial treatment of synovial plica syndrome typically includes conservative methods such as physical therapy, emphasizing stretching and strengthening exercises. Stretching enhances tissue pliability, while strengthening knee extensors is vital, as these muscles help prevent the plica from being pinched during knee movements.⁴ Limiting aggravating activities involving repetitive knee flexion and extension is also crucial.
Anti-inflammatory interventions include nonsteroidal anti-inflammatory drugs (NSAIDs), iontophoresis, and phonophoresis. If conservative measures fail, intra-articular corticosteroid injections may be considered, with surgical removal of the plica as a last resort.
Role of the Massage Therapist
Currently, no research specifically evaluates massage therapy for plica syndrome. However, the absence of studies does not negate the potential benefits of massage interventions. Massage has demonstrated effectiveness in managing soft-tissue fibrosis in various conditions. Considering that plica syndrome involves fibrosis of the synovial folds, massage may enhance tissue mobility, particularly in cases of fibrotic or calcified plicae.
Manual interventions might include gently pushing the patella laterally while applying friction massage to the medial tibiofemoral joint region and beneath the patella. Deep friction techniques can also be beneficial for other medial knee areas.
Furthermore, massage supports proper muscle tone and biomechanical balance in the VMO and distal quadriceps, reducing inappropriate tension in the knee capsule. As long as massage pressure remains within normal therapeutic limits, no contraindications are evident. In fact, massage therapy may decrease the likelihood of needing surgical intervention.
Massage could effectively complement conservative treatments like stretching and exercise. This condition represents an excellent opportunity for further research into massage therapy applications.
References
- Sznajderman T, Smorgick Y, Lindner D, Beer Y, Agar G. Medial plica syndrome. Isr Med Assoc J. 2009;11(1):54-57.
- Karaman İ, Güney A, Gürbüz K, Bilal Ö, Güney B. Calcific mediopatellar plica: a case report. Eklem Hast ve Cerrahisi (Jt Dis Relat Surg). 2013;24(2):117-120.
- Magee D. Orthopedic Physical Assessment. 6th ed. Philadelphia: W.B. Saunders; 2013.
- Camanho GL. Treatment of pathological synovial plicae of the knee.

